Degenerative Disc Disease
What is Degenerative Disc Disease?
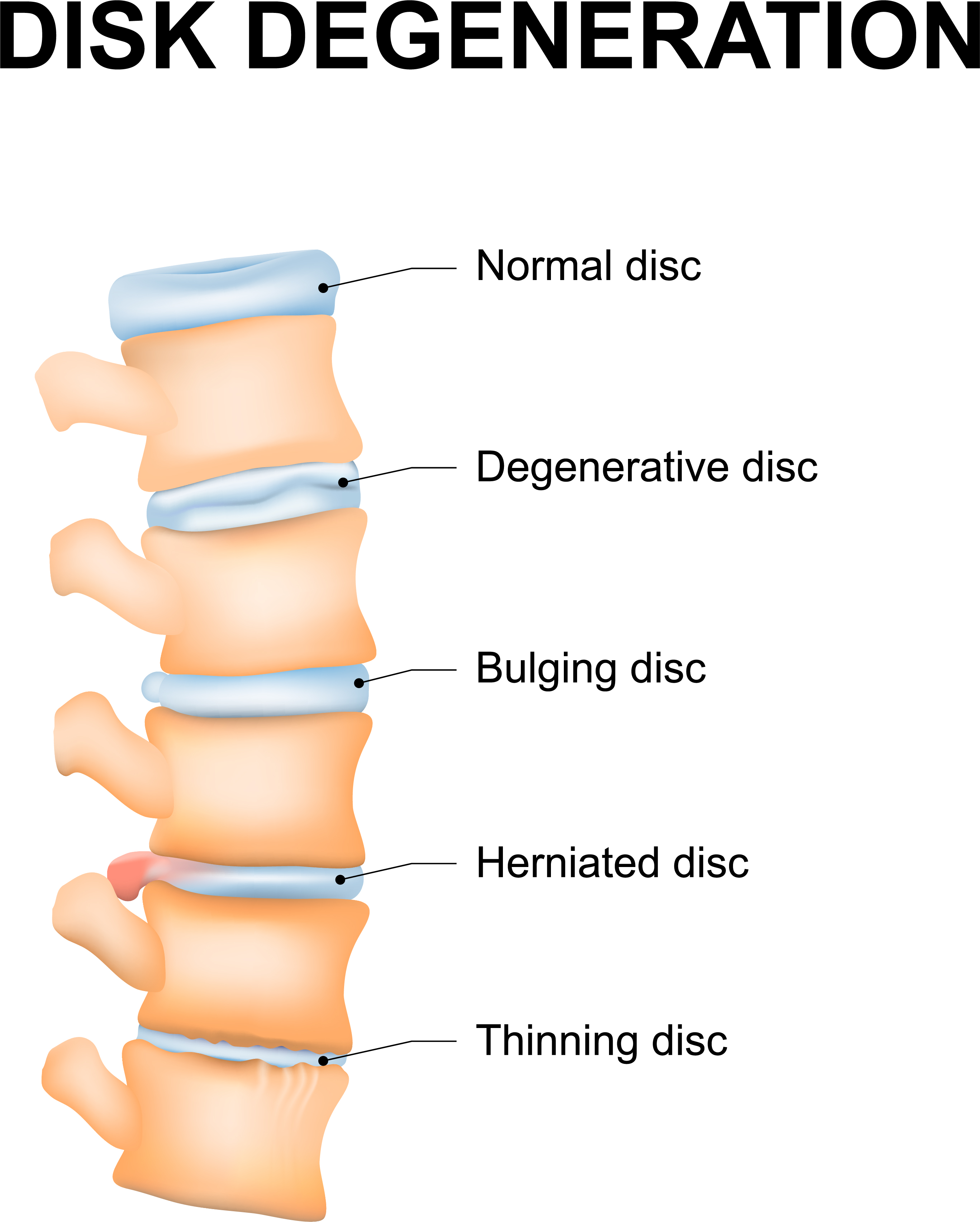
Aging causes disks to lose their water content which causes shrinkage, reduced sponginess, and loss of height. This means the vertebrae are closer together and can hinder certain movements or cause pain with different activities. The nerves that come off the spinal cord can become compressed or pinched. Overall, there is less shock absorption especially with walking, running, or jumping. Lifting heavy items incorrectly by not using the legs, twisting while lifting, and trauma can all damage the disks. Degenerative disc disease is broken down into three stages: dysfunction, instability, and restabilization or auto-fusion. Each stage has associated signs, symptoms, and duration.
Patient Education Video
What Causes Degenerative Disc Disease?
Obesity and being overweight greatly accelerates the process of disc degeneration and severity but aging itself is thought to be the primary cause. The rate of degeneration seems to be the only other variable. Besides decreased water and proteoglycan content, there is an increase in collagen levels. Other conditions such as alignment problems like spinal scoliosis, facet joint arthritis, history of trauma, and genes may all play a role.
What are the Symptoms?
Dysfunction Stage Tears and separation of the disc endplates, cartilage destruction, and a synovial inflammatory reaction can cause low back pain, neck pain, pain with motion. The pain can be located at a specific site or referred to other areas where the nerves supply sensory and motor control. Contracted muscles, tenderness at the site, decreased mobility, and pain when extending the neck or back are early signs and symptoms, but the neurologic exam is normal in most cases.
Instability Stage At this stage, there is resorption of the disc which decreases its height. The capsules around the facets become lax and may sublux (slide over) the other vertebrae. The symptoms include pain when standing after sitting, a 'catch' in the back, a sensation of swaying. The result is abnormal movements to counteract these abnormal sensations. Inflammatory chemicals called cytokines are released which aggravate the condition.
Restabilization or “Auto-Fusion” A natural reaction to Degenerative Disc Disease is that the edges of the vertebrae will develop growths by calcification of the ligaments, which results in gradual grow of adjacent vertebrae towards the each other and eventually in rare cases, the two vertebrae fuse. The low back pain may decrease in severity, but the muscles are still tender and stiff while the shape of the spine changes and overall movement is limited. Problems walking, tingling, numbness, or pain in the legs and buttocks are other generalized symptoms.
Instability Stage At this stage, there is resorption of the disc which decreases its height. The capsules around the facets become lax and may sublux (slide over) the other vertebrae. The symptoms include pain when standing after sitting, a 'catch' in the back, a sensation of swaying. The result is abnormal movements to counteract these abnormal sensations. Inflammatory chemicals called cytokines are released which aggravate the condition.
Restabilization or “Auto-Fusion” A natural reaction to Degenerative Disc Disease is that the edges of the vertebrae will develop growths by calcification of the ligaments, which results in gradual grow of adjacent vertebrae towards the each other and eventually in rare cases, the two vertebrae fuse. The low back pain may decrease in severity, but the muscles are still tender and stiff while the shape of the spine changes and overall movement is limited. Problems walking, tingling, numbness, or pain in the legs and buttocks are other generalized symptoms.
How is Degenerative Disc Disease Diagnosed?
Besides a history and physical exam that focuses on muscle strength, sensory loss, range of motion, and reflexes, MRI can diagnose both contained and non-contained disk herniations described as migrated disks, extruded disks, or protruded disks. MRI is also useful for categorizing free-fragment disk herniations from simple bulging to extruded disks. CT can be useful in herniation diagnosis if MRI is not available if contrast is used. There are some diagnostic tests that can also be therapeutic. Transforaminal selective nerve blocks (SNRBs) can help determine which specific nerve root is affected. Numbing medication and contrast material are used to numb the area that the nerve supplies under real-time guidance. This is especially useful when multiple levels are affected.
How is Degenerative Disc Disease Treated?
Initial treatment includes education, medications, physical exercise and therapy, and injections. Swimming is an excellent choice for these patients due to natural traction or decompression lengthening the spine. NSAIDs, muscle relaxants, and analgesics are the mainstay of medical treatment. Biofeedback, heating pads, electrical stimulation, and relaxation techniques are all beneficial. Epidural steroid injections can produce long-term relief in certain individuals especially if combined with morphine.
If a patient has exhausted conservative treatments for 6-12 months with persisting symptoms and reduced quality of life, they may consider elective surgery such as Artificial Disc Replacement (ADR) also referred to as Total Disc Replacement (TDR). However, surgery is mandatory in the case of increasing neurological deficits (drop-foot) caused by associated nerve compression, if the bowels or bladder are affected, or a condition known as cauda equina syndrome arises.
When the cervical or neck disks are compressed, early surgery (within six months) can lessen the progression. Patients with significant neurologic symptoms (myelopathy) who undergo surgery show significant improvement.
If a patient has exhausted conservative treatments for 6-12 months with persisting symptoms and reduced quality of life, they may consider elective surgery such as Artificial Disc Replacement (ADR) also referred to as Total Disc Replacement (TDR). However, surgery is mandatory in the case of increasing neurological deficits (drop-foot) caused by associated nerve compression, if the bowels or bladder are affected, or a condition known as cauda equina syndrome arises.
When the cervical or neck disks are compressed, early surgery (within six months) can lessen the progression. Patients with significant neurologic symptoms (myelopathy) who undergo surgery show significant improvement.
Surgery & Treatment for Degenerative Disc Disease
At Spine Connection we have regenerative and surgical treatments for all spine conditions. As every case is unique we encourage you to receive and compare opinions from our Neurosurgeon and Orthopedic Spine Specialists. We are here to help.
Begin My Assessment
Ask Our Doctors
Join Our Youtube Channel
Watch videos showcasing the latest technologies and surgery techniques, and keep up to date with patient stories from around the globe.