- Deep, achy joint pain worsened with use
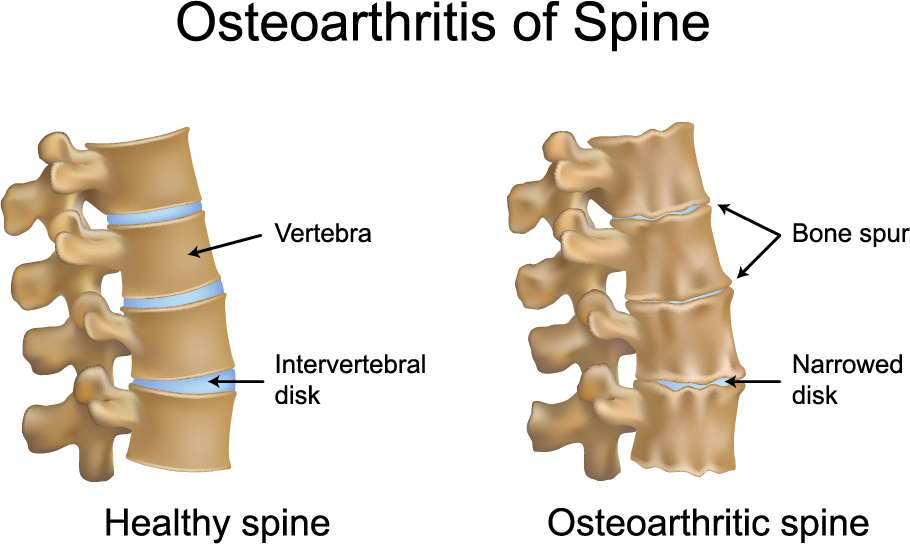
- Reduced flexibility and a cracking or grinding sound with joint movements
- Stiffness especially morning joint stiffness that lasts about 30 minutes
- Tenderness to touch
- Bone spurs or extra bone growth that stick out of the joints
Osteoarthritis
What is Osteoarthritis?
Osteoarthritis (OA) is a common type of arthritic joint disease that affects more than 30 million individuals in the United States. It is the result of degeneration of the hyaline cartilage of the joints that contain fluid but includes the entire joint complex including the bone and membrane surrounding the joint or synovium. The hands, hips, and knees are most commonly affected, but any joints or bones can be affected including the spine. The disease is considered progressive and is divided into three stages. The subsets of primary osteoarthritis are categorized as primary generalized osteoarthritis (PGOA), erosive osteoarthritis, and chondromalacia patellae (knee).
Stage 1 –
Proteins in the cartilage break down
Stage 2 –
Erosion of the cartilage's surface develops that releases protein metabolites and collagen into the synovial (joint) fluid
Stage 3 –
These breakdown products cause an inflammatory response that contributes to further cartilage breakdown over time
What are the Symptoms?
Symptoms of osteoarthritis include the following:
Osteoarthritis of the Hand
There are three joints in the fingers that can be affected with OA: distal which is near tips of fingers, middle, and the connection between the finger and the hand. The distal joints are most commonly affected as well as the base of the thumb. Bumps around the joints known as Heberden nodes are the result of bone spurs. Inflammatory changes as seen on X-Rays are less common in the hand compared to other joints such as the knees and hips.
Hand osteoarthritis has been classified as follows:
Hand osteoarthritis has been classified as follows:
- Erosive (worst cases)
- Thumb base
- Finger joints only (with or without nodes)
- Widespread hand
What Causes Osteoarthritis?
Joints that are subjected to daily stress especially the weight-bearing joints such as the ankle, hips, knees and lower spine are particularly susceptible. Most experts believe that breakdown of the articular cartilage is a result of excessive use and excessive pressure/weight applied to the joint. The joints that have previously been injured are also at risk. Joint composition changes as a result of excessive and repetitive external forces, which further accelerate the process. Other factors include
How is it Diagnosed?
Diagnosing OA does not depend on a specific blood test. Sometimes in severe erosive cases of OA, the erythrocyte sedimentation rate (ESR) may be elevated. Aspirating the synovial fluid may show a white blood cell (WBC) count below 2000/µL.
Plain Radiography: Plain X-Rays are a quick and cost-effective ways to diagnose OA especially with the load bearing joints such as the hip, knees, ankles and spine. X-Rays may show loss of joint-space, bony scaring, and cyst formation. An MRI can evaluate cartilage and other soft tissues around the joints better than X-Rays, including collections of fluid around the joints
Arthrocentesis: Aspirating joint synovial fluid can help exclude inflammatory arthritis, infection, or crystal causes of arthritis like gout. Arthrocentesis is done once other causes of arthritis are ruled out.
- Age
- Obesity
- Trauma/repetitive use
- Genetics
- Reduced levels of sex hormones
- Muscle weakness
- Infection
- Gout
- Previous inflammatory arthritis
- Inherited metabolic causes
- Hemoglobinopathies
- Neurological disorders
- Underlying bone malformations (eg, congenital hip dislocation)
- Disorders or diseases of bone
- Previous surgical procedures
- Diabetes mellitus
Plain Radiography: Plain X-Rays are a quick and cost-effective ways to diagnose OA especially with the load bearing joints such as the hip, knees, ankles and spine. X-Rays may show loss of joint-space, bony scaring, and cyst formation. An MRI can evaluate cartilage and other soft tissues around the joints better than X-Rays, including collections of fluid around the joints
Arthrocentesis: Aspirating joint synovial fluid can help exclude inflammatory arthritis, infection, or crystal causes of arthritis like gout. Arthrocentesis is done once other causes of arthritis are ruled out.
How is Osteoarthritis Treated?
Nonpharmacologic interventions are the mainstay of osteoarthritis therapy and include the following:
Pharmacologic management: Hand therapy medications include topical capsaicin, topical NSAIDs, oral NSAIDs, and Tramadol. Knee treatment includes Acetaminophen, oral NSAIDs, topical NSAIDs, Tramadol, and injections of steroids into the joint. Hips can be treated with everything previously listed except for topical capsaicin and topical NSAIDs.
Regenerative Treatment: Stem Cell Regeneration is an experimental and developing treatment for Osteoarthritis. Targeted cell therapy can lead to repair and regeneration of the damaged joints, as well as inhibition of the inflammatory effect that causes ongoing OA.
Surgical procedures: In the peripheral joints, surgery for osteoarthritis usually includes minimally invasive surgeries keyhole surgeries, including the opening of the joint capsule, and repair of the damaged joint. In the spine, surgery can vary on a case-by-case basis according to the damage caused, symptoms, and patient quality of life.
- Patient education and dietary changes
- Topical application of heat and cold
- Weight loss
- Exercise
- Physical therapy
- Occupational therapy
- Reducing stress in certain joints (eg, knee, hip)
Pharmacologic management: Hand therapy medications include topical capsaicin, topical NSAIDs, oral NSAIDs, and Tramadol. Knee treatment includes Acetaminophen, oral NSAIDs, topical NSAIDs, Tramadol, and injections of steroids into the joint. Hips can be treated with everything previously listed except for topical capsaicin and topical NSAIDs.
Regenerative Treatment: Stem Cell Regeneration is an experimental and developing treatment for Osteoarthritis. Targeted cell therapy can lead to repair and regeneration of the damaged joints, as well as inhibition of the inflammatory effect that causes ongoing OA.
Surgical procedures: In the peripheral joints, surgery for osteoarthritis usually includes minimally invasive surgeries keyhole surgeries, including the opening of the joint capsule, and repair of the damaged joint. In the spine, surgery can vary on a case-by-case basis according to the damage caused, symptoms, and patient quality of life.
Surgery & Treatment for Osteoarthritis
At Spine Connection we have regenerative and surgical treatments for all spine conditions. As every case is unique we encourage you to receive and compare opinions from our Neurosurgeon and Orthopedic Spine Specialists. We are here to help.
Begin My Assessment
Ask Our Doctors
Join Our Youtube Channel
Watch videos showcasing the latest technologies and surgery techniques, and keep up to date with patient stories from around the globe.