- 1. They want to try advanced cell based therapies
- 2. They have early stage damage and want to avoid or put off invasive surgery
- 3. They are not fit for invasive surgery but are in pain and still need treatment
- 4. They want to exhaust all conservative therapies before considering invasive surgery
- 5. They have pain after a previous spine surgery and are not a candidate for more surgery
- 6. Their spine damage is caused by underlying systemic disease such as Ankylosing Spondylitis (AS) or Rheumatoid Arthritis (RA) and they want systemic treatments targeting this
Stem Cell Therapy
for Spine Damage
Advanced Non-Surgical Treatment
If you are suffering with spine pain and do not want surgery or cannot have surgery, then advanced regenerative stem cell therapies may be suitable. Regenerative medicine has improved dramatically in the last 10 years, and when high-end providers of stem cell therapies come together with informed patients, then very good outcomes become possible.
Spine Connection patients can receive non-invasive stem cell treatment at one of the most advanced facilities in South-East Asia, with unlimited access to new technologies as they become available.
Spine Connection patients can receive non-invasive stem cell treatment at one of the most advanced facilities in South-East Asia, with unlimited access to new technologies as they become available.
Spine patients consider stem cell regeneration because:
It’s important to mention
At this time stem cell treatments and alternative medical treatments are considered experimental and are not approved by the U.S. FDA or other government regulatory agencies as the standard of care for any condition or disease. However this does not imply the lack of effectiveness, and our priority is to manage patient expectations for all regenerative cell therapies.
1What are Stem Cells and how do they work?
Stem Cells are unspecialized or blank cells with no specific function. When required, they respond to signals and change from blank to specialised cells in a process called differentiation.
Within the human body the stem cells that act as an internal repair system to repair and rebuild damaged tissues are called Mesenchymal Stem Cells (MSC).
Under ideal conditions a patient’s own MSCs would respond to damage and healing would occur. Factors that affect natural stem cell response include fitness of the patient, age, and the level of free radicals in the body.
Within the human body the stem cells that act as an internal repair system to repair and rebuild damaged tissues are called Mesenchymal Stem Cells (MSC).
Relative to Spine patients, MSCs can become:
- 1. Neuronal: Repair nerve tissue.
- 2. Myocytes: Repair muscle tissue.
- 3. Osteoblasts: Repair and grow bone tissue.
- 4. Chondrocytes: Repair and generate cartilage.
Under ideal conditions a patient’s own MSCs would respond to damage and healing would occur. Factors that affect natural stem cell response include fitness of the patient, age, and the level of free radicals in the body.
Other Benefits of Mesenchymal Stem Cells for Spine Patients
- 1. Well-Characterized: Mesenchymal stem cells are a well-characterized population of adult stem cells, with over 36,000 scientific articles published about them.
- 2. Non-Controversial: Mesenchymal stem cells avoid the ethical issues of embryonic stem cells, as they can be derived from sources that include adult bone marrow, adipose tissue and donated umbilical cord blood.
- 3. Diverse Differentiation Potential: Mesenchymal stem cells can form a variety of cell types in the laboratory, including those of both intra- and extra-mesenchymal lineage. These cell types include: fat (adipocytes), bone (osteoblasts), skin (dermal cells), nerve (neural cells), cartilage (chondrocytes), muscle (skeletal myocytes), tendons (tenocytes), marrow stroma, ligaments, and more.
- 4. Ease of Growth in Culture: Advanced knowledge exists for how to grow Mesenchymal stem cells in culture, including protocols for isolation, expansion, and differentiation.
- 5. Flexible Propagation: Mesenchymal stem cells can be grown and propagated in culture for extended periods, without losing differentiation potential.
- 6. Role as Regulatory Cells: Mesenchymal stem cells synthesize and secrete a variety of macromolecules that are known regulators of hematopoietic and bone-resorbing cells.
- 7. Favourable Immune Status: Mesenchymal stem cells lack the co-stimulatory molecules of the B7 family that are required to initiate an immune response. This allows the administration of MSC preparations across MHC barriers without concern for immunological rejection or the need for immunosuppression, making Mesenchymal stem cells a universal stem cells source.

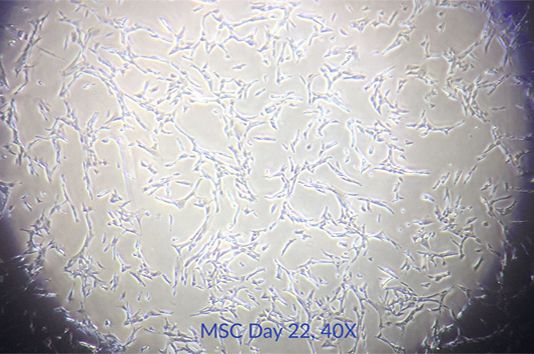

Visualise Mesenchymal Stem Cells expanding in culture.
2Which Stem Cell sources are most suitable?
(Adipose Vs. Bone Marrow Vs. Cord Tissue)
Stem Cells can be sourced from multiple areas of the human body. When treating patients, doctors commonly use stem cells procured from your fat (adipose), bone marrow or blood.
Today you will find many doctors and clinics treating joint and spine conditions with autologous stem cells from their adipose (fat) tissue via liposuction or from bone marrow. The term autologous means that the cells are harvested from the patient’s own adult body.
The procedures required to extract adipose or bone marrow cells often involve invasive and unnecessary cell harvesting surgery. The trauma and inflammation caused at the site of cell harvesting can also inhibit stem cell therapy outcomes, by distracting stem cells away from the focus area of damage - where they are needed most.
“Our partner clinics and laboratories prefer Umbilical Cord tissue as a source of Stem Cells to treat spinal conditions.”
Benefits of Umbilical Cord Tissue for Stem Cell Spine Regeneration
Umbilical cord tissue comes from the donated umbilical cord just after birth. It represents a unique, easy accessible and noncontroversial source of early stem cells that can be readily processed for therapeutic use.
Naturally, umbilical cord MSC’s must prepare and facilitate the most intensive growth and development period of the human lifecycle: from birth until 3 years.
Cord cells have the potential for increased therapeutic effect compared to autologous stem cells taken from an adult’s own body, particularly a body requiring repair because it has become ineffective at managing its own recovery and regeneration. Our partner clinics and laboratories have visualised key differences between Umbilical Cord Mesenchymal Stem Cells and Adipose Fat / Bone Marrow derived sources:
The added benefit for the patient is that no invasive surgery and trauma is required to harvest Umbilical Cord derived Stem Cells. They are prepared within the cell laboratory and injected intravenously and into the spine treatment areas by experienced doctors and specialists. Supportive therapies are also used to achieve the best clinical outcome.
Naturally, umbilical cord MSC’s must prepare and facilitate the most intensive growth and development period of the human lifecycle: from birth until 3 years.
Have you noticed how a grazed knee or other injury tends to heal faster for a young child compared to an adult?
Cord cells have the potential for increased therapeutic effect compared to autologous stem cells taken from an adult’s own body, particularly a body requiring repair because it has become ineffective at managing its own recovery and regeneration. Our partner clinics and laboratories have visualised key differences between Umbilical Cord Mesenchymal Stem Cells and Adipose Fat / Bone Marrow derived sources:
- 1. Umbilical cord MSCs appear to lack some immune properties compared with adult stem cells (the immune system doesn’t recognise them to induce an immune response).
- 2. Umbilical cord MSC’s lack class II HLA, whereas adult mesenchymal stem cells express these antigens. This is very important in facilitating "acceptance" of transplanted cells.
- 3. Umbilical cord mesenchymal stem cells express a higher range and level of growth factors & specific cytokines when compared to adult mesenchymal stem cells.
The added benefit for the patient is that no invasive surgery and trauma is required to harvest Umbilical Cord derived Stem Cells. They are prepared within the cell laboratory and injected intravenously and into the spine treatment areas by experienced doctors and specialists. Supportive therapies are also used to achieve the best clinical outcome.



Treatments are provided in state of the art facilities with in-house Laboratories and cryogenic banking
3Difference between Young and Old Stem Cells
Now that we have discussed the clinical benefits of Umbilical Cord derived Stem Cells over Adipose and Bone Marrow sourced cells, let’s look at the difference between young and old cells.
The difference between young and old MSCs in morphology, cell surface antigen phenotype, proliferation, gene expression and immunomodulatory ability are proven.
When you expand the numbers of young mesenchymal stem cells into further passage, senescent MSCs display a characteristically enlarged and flattened morphology and different gene expression profiles.
Human mesenchymal stem cells have insufficient telomerase activity to overcome progressive telomere shortening caused by end-replication problems and oxidative stress associated with higher rates of culture.
The difference between young and old MSCs in morphology, cell surface antigen phenotype, proliferation, gene expression and immunomodulatory ability are proven.
When you expand the numbers of young mesenchymal stem cells into further passage, senescent MSCs display a characteristically enlarged and flattened morphology and different gene expression profiles.
Human mesenchymal stem cells have insufficient telomerase activity to overcome progressive telomere shortening caused by end-replication problems and oxidative stress associated with higher rates of culture.
“In short, early passage cells are more powerful and have greater therapeutic potential.”
Optimising Mesenchymal Stem Cell Culture for Therapeutic Use:
Over a 2-3 week period MSCs can rapidly proliferate achieving potentially thousands of fold expanded cells.
However, inappropriate expansion reduces the quality of the cells. Therapeutic properties of the stem cells will be lost during prolonged culture, for example, the cardio protective effect of mesenchymal stem cells grown to Passage 3 is significantly reduced compared to Passage 1 mesenchymal stem cells.
In our partner laboratories as a standard, the most important parameter they use for determining clinical cell culture is using population doubling time. Population doubling time refers to the number of times two-fold increase (doubling) of the cells in culture. Population doubling time directly correlates with replicative senescence, loss of potency and genomic instability. Mesenchymal stem cell senescence is reported in cultures with population doubling time from 10-40. This worsens and becomes shorter every time the cell culture is forced through another passage.
Most other stem cell labs continue to culture cells into Passage 3. By this time the original culture flask has filled its surface of around 80% and a portion of the cells are then seeded into a new culture flask to grow further. Each passage can have between 10-40 doublings depending on starting volume of cells. So in theory cells which have been cultured to Passage 3 could have undergone 30-120 doublings.
Thus as a quality guarantee protocol, our partner SC21 laboratories maintain Passage 1 culture with a restriction on doubling of 5-10 times. This maintains the stem cell naivety status and higher activity levels to deliver the best clinical outcome possible.
However, inappropriate expansion reduces the quality of the cells. Therapeutic properties of the stem cells will be lost during prolonged culture, for example, the cardio protective effect of mesenchymal stem cells grown to Passage 3 is significantly reduced compared to Passage 1 mesenchymal stem cells.
“A passage is when a portion of cells are transferred into new flasks to grow”
In our partner laboratories as a standard, the most important parameter they use for determining clinical cell culture is using population doubling time. Population doubling time refers to the number of times two-fold increase (doubling) of the cells in culture. Population doubling time directly correlates with replicative senescence, loss of potency and genomic instability. Mesenchymal stem cell senescence is reported in cultures with population doubling time from 10-40. This worsens and becomes shorter every time the cell culture is forced through another passage.
Most other stem cell labs continue to culture cells into Passage 3. By this time the original culture flask has filled its surface of around 80% and a portion of the cells are then seeded into a new culture flask to grow further. Each passage can have between 10-40 doublings depending on starting volume of cells. So in theory cells which have been cultured to Passage 3 could have undergone 30-120 doublings.
Thus as a quality guarantee protocol, our partner SC21 laboratories maintain Passage 1 culture with a restriction on doubling of 5-10 times. This maintains the stem cell naivety status and higher activity levels to deliver the best clinical outcome possible.



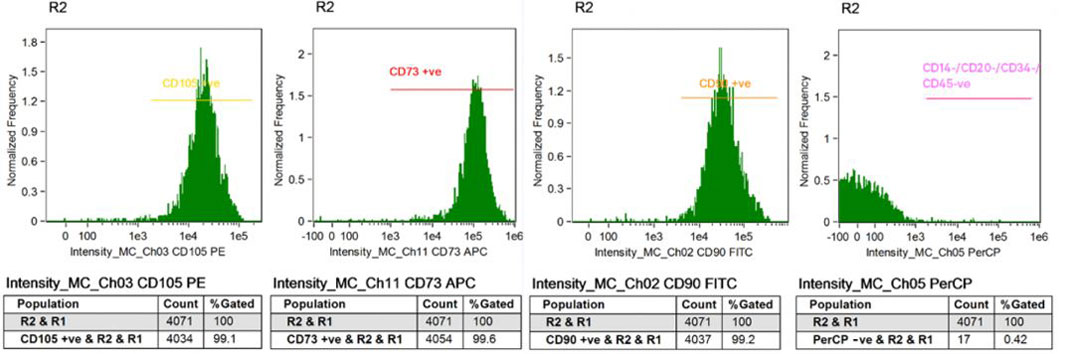
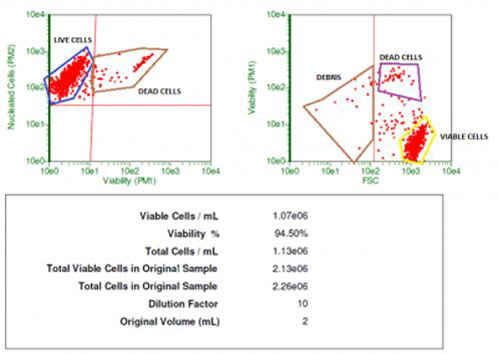
Patients deserve accurate reporting showing quality control and proof of viability for the Stem Cells being used to treat their condition. Our partner SC21 in-house laboratories use Laser Flow Cytometry and other protocols to guarantee this process from ‘A-Z’.
4Which Spine Conditions can be treated with Stem Cells?
- 1Arthritis and Facet Joint Damage
Facet Arthropathy (FA) is an arthritic condition of the facet joints, and this can be a major cause of back pain. In a healthy spine these joints allow for bending, twisting, and alignment. Facet damage can be caused by a traumatic injury, or by wear-and-tear over time. Certain spinal conditions can affect the facet joints, including types of arthritis and Degenerative Disc Disease (DDD), where a dehydrated and dysfunctional disc places extra stress on the facet joint.

SC21 Recommended Treatment Program:
The treatment program for Arthritis and Facet Joint Damage involves systemic (IV) and paraspinal administration of Passage 1 Cord Stem Cells for maximum clinical benefit.
50-300 Million Cells administered over a 3-14 day period, depending on the severity of your condition and budget.
Follow Up: If you respond well to treatment, with improvement in mobility, pain levels, nerve function, X-Ray/MRI images or overall quality of life, then follow up treatments may be beneficial.
Supportive therapies such as RNA Therapy, IV Laser, IV Oxygen, IV Nutrition, Shockwave Therapy, Physiotherapy and Spinal Laser Therapy are administered alongside stem cell treatment for Chronic Back Pain for an enhanced outcome
- 2Chronic Back Pain
Chronic Back Pain can be caused by musculoskeletal spine or nerve damage, from a traumatic injury or general wear-and-tear over time. It can also be brought on after a previous spine surgery.
Patients suffering with chronic back pain usually consider non-invasive therapies such as physiotherapy, chiropractic, deep tissue massage and medications before considering any spine surgery options. Stem cell therapy is also a non-invasive treatment for this condition.
Sometimes patients are not suitable for spine surgery due to their spine damage being too complex/severe, presence of underlying conditions, or unsuitability for anaesthetics required for surgery. These are both scenarios where patients may consider regenerative stem cell treatment for their back.
SC21 Recommended Treatment Program:
The treatment program for chronic back pain involves systemic (IV) and paraspinal administration of Passage 1 Cord Stem Cells for maximum clinical benefit.
50-300 Million Cells administered over a 3-14 day period, depending on the severity of your condition and budget.
If you respond well to treatment, with improvement in mobility, pain levels, nerve function, X-Ray/MRI images or overall quality of life, then follow up treatments may be beneficial.
Supportive therapies such as RNA Therapy, IV Laser, IV Oxygen, IV Nutrition, Shockwave Therapy, Physiotherapy and Spinal Laser Therapy are administered alongside stem cell treatment for Chronic Back Pain for an enhanced outcome.
- 3Rheumatoid Arthritis (RA)
Rheumatoid arthritis (RA) is an autoimmune disease that causes chronic inflammation of the joints. Symptoms are triggered when antibodies attack the synovial joint fluid, causing chronic inflammation, joint damage and deformity. ‘Passage 1’ Umbilical Cord derived Stem Cells are active in immune modulation, which is important for Rheumatoid Arthritis (RA) sufferers. The regenerative and anti-inflammatory functions of these cells can also benefit patients.
There is no known cure for rheumatoid arthritis. To date, the goal of stem cell treatment in RA is to reduce joint inflammation and pain, maximize joint function, and prevent joint destruction and deformity. Early medical intervention before significant joint damage has occurred has been shown to be important in improving outcomes.

SC21 Recommended Treatment Program:
The treatment program for Rheumatoid Arthritis involves systemic (IV) and paraspinal administration of ‘Passage 1’ Cord Stem Cells for maximum clinical benefit.
50-300+ Million Cells administered over a 3-14 day period, depending on the severity of your condition and budget. Due to the systemic nature of RA, follow up sessions are advised, with results measured over a period of months.
If you respond well to treatment, with improvement in mobility, pain levels, nerve function, X-Ray/MRI images or overall quality of life, then follow up treatments may be beneficial.
Supportive therapies such as RNA Therapy, IV Laser, IV Oxygen, IV Nutrition, Shockwave Therapy, Physiotherapy and Spinal Laser Therapy are administered alongside stem cell treatment for Rheumatoid Arthritis (RA) for an enhanced outcome.
- 4Ankylosing Spondylitis (AS)
Ankylosing spondylitis is a type of arthritis that affects the spine. Ankylosing spondylitis symptoms include pain and stiffness from the neck down to the lower back. The spine's bones (vertebrae) fuse together, resulting in a rigid spine. Like in Rheumatoid Arthritis, early diagnosis and treatment helps control pain and stiffness and may reduce or prevent significant deformity. Although the exact cause of AS is unknown, we do know that genetics play a key role in the disease.
Advanced regenerative therapies can deliver promising results for damaged spinal joints and systemic autoimmune regulation, reducing the ongoing inflammatory cycle AS patients suffer from.
There is no known cure for Ankylosing Spondylitis. To date, the goal of stem cell treatment in AS is to reduce joint inflammation and pain, maximize joint function, and prevent joint destruction and deformity. With early diagnosis and proper medical care, AS is manageable.
SC21 Recommended Treatment Program:
The treatment program for Ankylosing Spondylitis involves systemic (IV) and paraspinal administration of ‘Passage 1’ Cord Stem Cells for maximum clinical benefit.
50-300+ Million Cells administered over a 3-14 day period, depending on the severity of your condition and budget. Due to the systemic nature of AS, follow up sessions are advised, with results measured over a period of months.
If you respond well to treatment, with improvement in mobility, pain levels, nerve function, X-Ray/MRI images or overall quality of life, then follow up treatments may be beneficial.
Supportive therapies such as RNA Therapy, IV Laser, IV Oxygen, IV Nutrition, Shockwave Therapy, Physiotherapy and Spinal Laser Therapy are administered alongside stem cell treatment for Ankylosing Spondylitis (AS) for an enhanced outcome.
- 5Spinal Cord Injury (SCI)
Spinal cord injury (SCI) is a serious form of trauma with enduring effects on the patient’s quality of life. This damage is usually caused by force, such as a motor vehicle accident, falling off a horse or diving into shallow water. Spinal cord damage can cause disturbances in bodily movement and function, and patients living with this condition show great determination and resolve in going about their day-to-day lives, usually with care and support from family and friends.
Spinal cord injuries fall into 2 categories:
- A Incomplete spinal cord injuries; the spinal cord is partially severed, the patient retains some functions depending on the degree of the injury. Some of the common types of partial spinal cord include anterior cord syndrome, central cord syndrome and brown-sequard syndrome.
- B Complete spinal cord injuries; this type occurs when the spinal cord is completely severed and there is no function below the level of injury.
When introduced into the Cerebral Spinal Fluid (CSF) via lumbar puncture, ‘Passage 1’ Cord Stem Cells have the ability to differentiate into nerve cells and assist with regrowth and repair of the damaged spinal cord at the site of injury.
The goal is that when combined with a physical rehabilitation program and supportive therapies, these newly reformed nerve pathways can learn to send signals to restore bodily movement and function.
Paraspinal and systemic IV administration of stem cells can also assist in rebuilding and strengthening of bone, muscle and other soft structures required for mobility.
While right now there is no guaranteed cure for this condition, every year we see exciting developments from SCI research groups around the world. The key objective of stem cell therapy is to provide a chance for improvement in movement, bodily function and quality of life.
SC21 Recommended Treatment Program:
The treatment program for Spinal Cord Injury involves systemic (IV), paraspinal and Cerebral Spinal Fluid (CSF) administration of ‘Passage 1’ Cord Stem Cells for maximum clinical benefit.
100-300 Million Cells administered over a 10-14 day period, depending on the severity of your condition and budget.
If you show improvement in mobility, pain levels, nerve function, MRI images or overall quality of life, then continued benefits may be achieved with further treatment. Results can be measured over a period of months
Supportive therapies such as RNA Therapy, IV Laser, IV Oxygen, IV Nutrition, Shockwave Therapy, Physiotherapy and Spinal Laser Therapy are administered alongside stem cell treatment for Spinal Cord Injury (SCI) for an enhanced outcome.
5. Supportive Therapies for
an Enhanced Outcome
Spine damage can be caused by a traumatic injury, wear-and-tear, or degenerative disease. If your body isn’t repairing itself like it was designed to, it can be because the damage is too great, or your body’s natural repair process is underperforming and needs help.
Introducing Passage 1 Cord Mesenchymal Stem Cells to the affected spine areas represents only half of the spine regeneration equation. The other half involves supportive therapies to assist the performance of the repair cells inside your body, creating an internal environment that’s conducive to growth and regeneration.
Introducing Passage 1 Cord Mesenchymal Stem Cells to the affected spine areas represents only half of the spine regeneration equation. The other half involves supportive therapies to assist the performance of the repair cells inside your body, creating an internal environment that’s conducive to growth and regeneration.
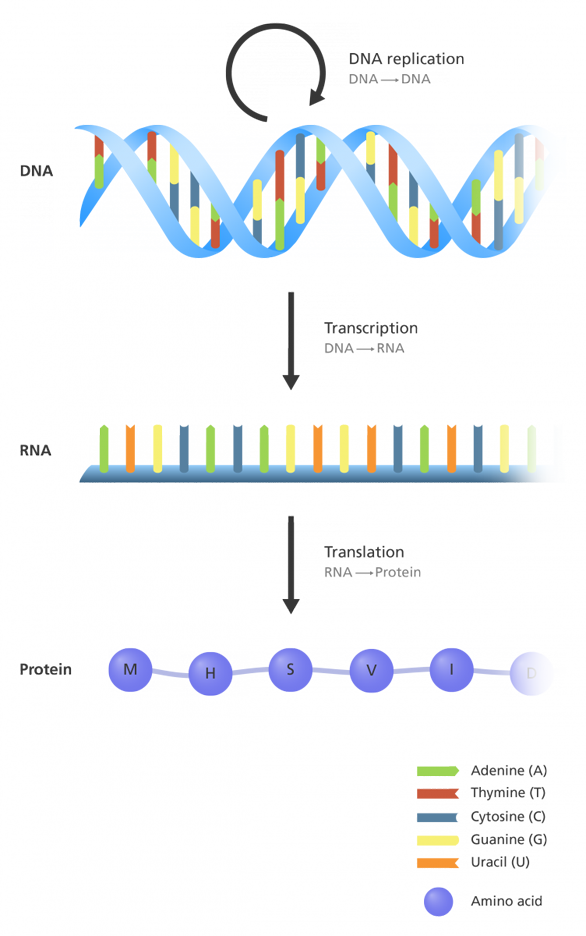
RNA Therapy
Ribonucleic Acid (RNA) is a nucleic acid present in all living cells. Messenger RNA is a type of RNA with the principal role of acting as messenger, carrying instructions from DNA to assemble amino acids into proteins.
Oligonucleotides are short RNA molecules. As well as being important in the biosynthesis of proteins, they have additional functions which contribute to the maintenance of healthy cell regulation and function. They can influence and regulate DNA synthesis, cell differentiation and immune properties.
Condition-specific oligonucleotides support rapid re-stimulation of reduced cell activity, increasing the potential for regeneration and restoration of damaged tissue.
Ribonucleic acids from the intervertebral disc, cartilage, synovia, placenta (bovine) and from yeast. This preparation is used in the supportive treatment of osteochondrosis, osteoporosis, arthrosis and osteoarthritis.
RNA Therapy is prescribed on a case-by-case basis and prescribed dosage are delivered intravenously during in-clinic stem cell therapy.
Oligonucleotides are short RNA molecules. As well as being important in the biosynthesis of proteins, they have additional functions which contribute to the maintenance of healthy cell regulation and function. They can influence and regulate DNA synthesis, cell differentiation and immune properties.
Condition-specific oligonucleotides support rapid re-stimulation of reduced cell activity, increasing the potential for regeneration and restoration of damaged tissue.
A condition-specific “OsteoRepair” RNA Treatment Set includes:
Ribonucleic acids from the intervertebral disc, cartilage, synovia, placenta (bovine) and from yeast. This preparation is used in the supportive treatment of osteochondrosis, osteoporosis, arthrosis and osteoarthritis.
RNA Therapy is prescribed on a case-by-case basis and prescribed dosage are delivered intravenously during in-clinic stem cell therapy.
Intravenous Nutrition Support
You are what you eat. Intravenous IV nutrition is a method of feeding vitamins, minerals, and other natural substances directly into a patient’s bloodstream. Bypassing the digestive system is the main advantage of IV nutrition. When substances are given orally they must be processed through the stomach and the intestines.
By directly administering nutrients to the body higher than normal blood levels can be achieved. These increased levels can provide an immediate therapeutic response by correcting deficiencies that may arise from a disease state. Scientific research has demonstrated that a variety of conditions can benefit from the use of IV nutrition.
All intravenous protocols offered have been thoroughly researched and have been shown to be effective in the treatment of certain conditions. By practicing this type of “evidence-based medicine” we can custom tailor our IV infusions to ensure maximal effectiveness combined with minimal side effects.
By directly administering nutrients to the body higher than normal blood levels can be achieved. These increased levels can provide an immediate therapeutic response by correcting deficiencies that may arise from a disease state. Scientific research has demonstrated that a variety of conditions can benefit from the use of IV nutrition.
IV Nutrition Infusions are important because:
- 1. Most people are not eating a diet rich in vitamins and minerals daily
- 2. Many people have compromised digestion and cannot properly absorb nutrients
- 3. Many vitamins and minerals act as pharmaceuticals at higher doses
All intravenous protocols offered have been thoroughly researched and have been shown to be effective in the treatment of certain conditions. By practicing this type of “evidence-based medicine” we can custom tailor our IV infusions to ensure maximal effectiveness combined with minimal side effects.
Intravenous Laser Therapy
Originating over 25 years ago, intravenous (in the vein) lasers are now used clinically to treat a range of medical conditions. Intravenous (IV) lasers are modern medical devices which are inserted through a standard needle attachment and into a vein in the arm or hand.
As the venous blood rushes over the tip of the needle, concentrated beams of laser at carefully tuned wavelengths drench the blood cells and the fluid plasma in a process called ‘intravenous irradiation’. This technology is now FDA-approved and patented by German Technology Company Weber Medical.
Doctors have published studies observing IV Laser Therapy can increase the oxygen carrying capacity of red blood cells, a scenario most important for repair and regeneration.
As the venous blood rushes over the tip of the needle, concentrated beams of laser at carefully tuned wavelengths drench the blood cells and the fluid plasma in a process called ‘intravenous irradiation’. This technology is now FDA-approved and patented by German Technology Company Weber Medical.
For patients undergoing stem cell treatment for spine damage:
Doctors have published studies observing IV Laser Therapy can increase the oxygen carrying capacity of red blood cells, a scenario most important for repair and regeneration.
Green Wave Length:
Increases Nitro Oxide, increases bonding of Haemoglobin & reduces blood viscosity.
Red Wave Length:
Increases ATP (energy) production in Mitochondria, stimulates metabolism and increases Stem Cell activity / Regeneration.
Blue Wave Length:
Anti-bacterial, anti-viral, anti-inflammatory and Immune function regularity.
Yellow Wave Length:
Stimulates mitochondrial respiratory chain at complex 2 cytochromes, has a detoxifying effect, and has an anti-depressive effect (in combination with hypericin).
Intravenous Oxygen Therapy
Oxygen is essential for life. Normally it is brought into the lungs via breathing, where it is transported by red blood cells to the entire body to be used as energy.
The application of medical oxygen was developed during more than 30 years of research by Dr. med. H. S. Regelsberger. In that time he developed a therapy allowing pure oxygen to be introduced to the body slowly and in a precise dosage, in low quantities, directly via the veins. This process is proven safe and without side effects.
It is shown that IV Oxygen Therapy produces a general improvement in oxygen availability, as well as increased cellular immunological resistance. Flow properties of blood and its elements of plasma and cells are improved, increase of oxygen into the tissue is increased, and blood Ph is normalised. Compared with hyperbaric oxygen therapy, IV Oxygen Therapy appears to have less side effects and likely has higher efficacy.
The application of medical oxygen was developed during more than 30 years of research by Dr. med. H. S. Regelsberger. In that time he developed a therapy allowing pure oxygen to be introduced to the body slowly and in a precise dosage, in low quantities, directly via the veins. This process is proven safe and without side effects.
It is shown that IV Oxygen Therapy produces a general improvement in oxygen availability, as well as increased cellular immunological resistance. Flow properties of blood and its elements of plasma and cells are improved, increase of oxygen into the tissue is increased, and blood Ph is normalised. Compared with hyperbaric oxygen therapy, IV Oxygen Therapy appears to have less side effects and likely has higher efficacy.
Shockwave Therapy
Shockwave therapy is used in orthopedics, physiotherapy and sports medicine. It is used for fast pain relief and to restore mobility. As a non-surgical therapy, it is designed to speed up recovery and cure various indications causing acute or chronic pain.
High-energy acoustic pulses used in shockwave therapy create micro traumas, which in-turn increase repair signals & activity in the target area. When stem cells are then introduced, they have an increased number of repair signals to home to and regenerate.
Shockwave therapy boosts cell metabolism in the pain region and increases blood circulation by stimulates the body’s intrinsic repair mechanisms. Damaged tissue gradually regenerates and as a result, eventually heals. Shockwave treatment is an ideal pain relief and mobility increasing therapy.
How Shockwave Therapy Works:
High-energy acoustic pulses used in shockwave therapy create micro traumas, which in-turn increase repair signals & activity in the target area. When stem cells are then introduced, they have an increased number of repair signals to home to and regenerate.
Shockwave therapy boosts cell metabolism in the pain region and increases blood circulation by stimulates the body’s intrinsic repair mechanisms. Damaged tissue gradually regenerates and as a result, eventually heals. Shockwave treatment is an ideal pain relief and mobility increasing therapy.
For patients with Spinal Damage:
Shockwave Therapy carries high energy to painful spots and myoskeletal tissues, promoting repair of the bones, tendons and other soft tissues.
Medical Action of Shockwave Therapy:
- - New Blood Vessel Formation
- - Reversal of Chronic Inflammation
- - Stimulation of Collagen Production
- - Dissolution of Calcified Fibroblasts
- - Dispersion of Pain Mediator
- - Release of Trigger Points

Physiotherapy
Physiotherapists are highly qualified health professionals who work closely with their patients to help them get better and stay well. They also work closely with doctors and other health clinicians to plan and manage treatment.
Using advanced techniques and evidence-based care, physiotherapists assess, diagnose, treat and prevent a wide range of health conditions and movement disorders. Physiotherapy helps repair damage, reduce stiffness and pain, increase mobility and improve quality of life.
Physiotherapy extends from health promotion to injury prevention, acute care, rehabilitation, maintenance of functional mobility, chronic disease management, patient and carer education and occupational health.
Using advanced techniques and evidence-based care, physiotherapists assess, diagnose, treat and prevent a wide range of health conditions and movement disorders. Physiotherapy helps repair damage, reduce stiffness and pain, increase mobility and improve quality of life.
Physiotherapy extends from health promotion to injury prevention, acute care, rehabilitation, maintenance of functional mobility, chronic disease management, patient and carer education and occupational health.

For patients with Spinal Damage:
Physiotherapy is a science-based profession and takes a ‘whole person’ approach to health and wellbeing, which includes the patient’s general lifestyle. While a spine patient is undergoing regenerative stem cell therapies, learning to move confidently again is part of the repair process.
The fundamental belief in physiotherapy is that patients should actively participate in their own care through education, awareness, empowerment and involvement. This ensures the patient can continue their daily exercise, strengthening and rehabilitation program as part of their new lifestyle, long after they return home.
Spinal Laser Therapy
Spinal laser therapy uses the same German FDA approved technology as Intravenous Laser Therapy we explained earlier. With this new technique, the so-called percutaneous interstitial laser therapy (with the use of a sterile catheter), allows the laser light to be used even deeper in the tissue, for treatment of damaged spine areas.
Using this technique, it is possible to achieve a penetration depth of up to 12 cm and improved therapeutic results can be obtained. Green and blue lasers which are normally absorbed on the surface of the tissue can be used to target deeper areas for anti-inflammatory benefits.
Using this technique, it is possible to achieve a penetration depth of up to 12 cm and improved therapeutic results can be obtained. Green and blue lasers which are normally absorbed on the surface of the tissue can be used to target deeper areas for anti-inflammatory benefits.
Application areas of interstitial laser therapy:
- - Chronic spinal illnesses
- - Slipped discs
- - Scar pain after slipped disc surgery
- - Spinal stenosis
- - Neural lesions
- - Deep tendinitis and strains
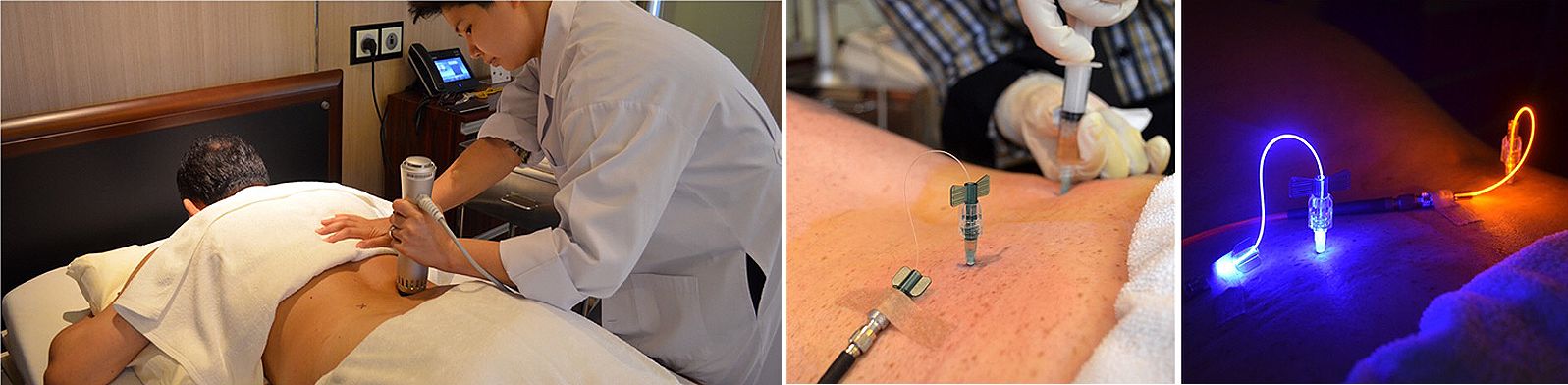
Visualise how spinal laser therapy is applied in a real patient case.
Join Our Youtube Channel
Watch videos showcasing the latest technologies and surgery techniques, and keep up to date with patient stories from around the globe.