Sciatica (Pinched Nerve)
What is Sciatica?
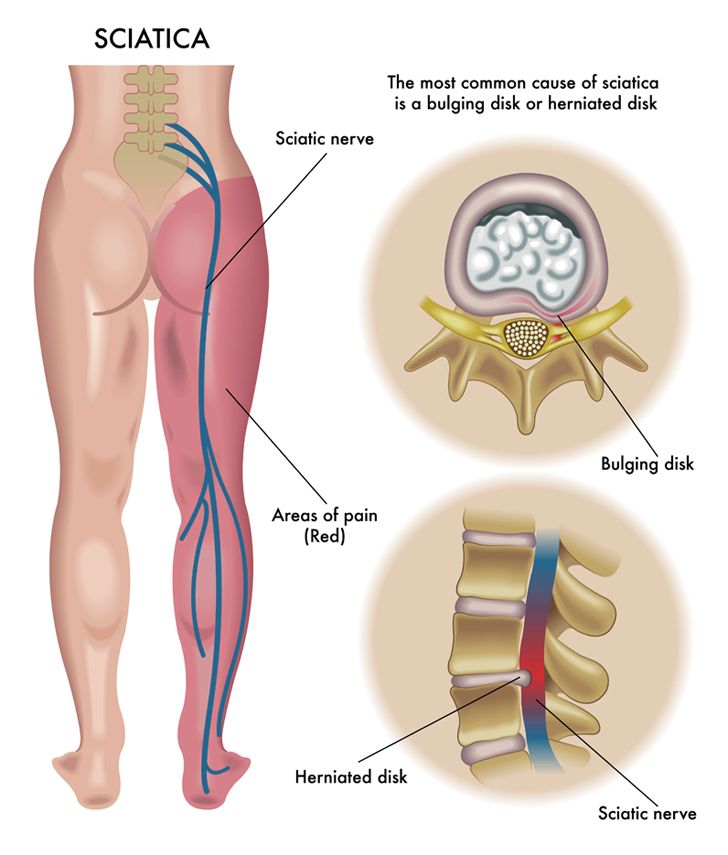
Sciatica is nerve pain that begins in the hip and deep in the buttocks and travels down the leg. The largest nerve that supplies the lower body is the sciatica nerve. It comes off the lower spinal cord (lumbar-sacral nerve roots) and dives behind an opening (obturator canal) in the pelvic bone before it branches off to supply the upper and lower legs and the feet.
The pain from sciatica comes from pressure and swelling that results in the nerve pressing against the bones of the pelvis or spinal column. Sciatica can cause neurological deficits such as weakness or numbness in the legs and feet.
Muscles that get pinched such as the piriformis muscle and internal obturator muscle can lead to the symptoms of sciatica. This muscle near the hip can be injured or damaged which causes swelling that leads to pain.
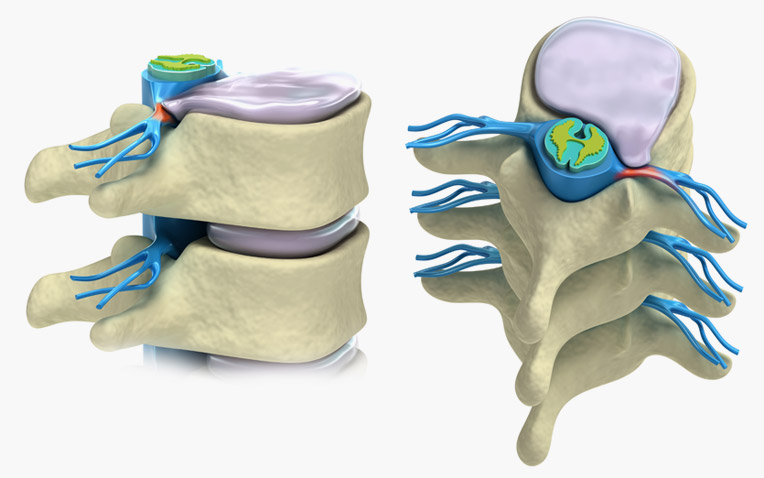
True sciatica happens when a herniated disc or osteoarthritic bone spurs compress one of the contributing roots of the sciatica nerve. This results in a ‘pinched nerve’. Sciatica is less common than other types of low back pain.
The pain from sciatica comes from pressure and swelling that results in the nerve pressing against the bones of the pelvis or spinal column. Sciatica can cause neurological deficits such as weakness or numbness in the legs and feet.
Muscles that get pinched such as the piriformis muscle and internal obturator muscle can lead to the symptoms of sciatica. This muscle near the hip can be injured or damaged which causes swelling that leads to pain.
True sciatica happens when a herniated disc or osteoarthritic bone spurs compress one of the contributing roots of the sciatica nerve. This results in a ‘pinched nerve’. Sciatica is less common than other types of low back pain.
Patient Education Video
What is Radiculopathy?
Radiculopathy is the medical term for sciatica and specifically describes pain, numbness, tingling, or weakness in any body area or muscle as a result of their respective nerve roots being compressed or injured. This can include a Herniated Disc, Spinal Stenosis or other lower spinal condition. The number of nerve roots involved varies but can involve both sides of the body or just one side.
What Causes Sciatica?
1. The first cause of sciatica is the result of a Herniated Disc. The intervertebral disc can become herniated as a result of being ruptured, bulging, or torn. If the bulging disc presses on a spinal nerve, then that area of the body that the nerve supplies will experience symptoms such as pain or throbbing. Most disc ruptures occur in a person who is in their 30s or 40s when the disc contents are a jelly-like substance.
2. The second cause is Degenerative Disc Disease (DDD) as a result of aging and excessive micromotion of the spine over time. Bone spurs contribute as well.
3. Isthmic Spondylolisthesis is a result of a small stress fracture that allows one disc to slip forward over another disc which can also pinch a nerve. As the spinal canal narrows as we age and arthritis sets in, sciatica can occur.
4. The sciatica nerve runs behind the piriformis muscle of the buttock. If that muscle gets irritated, it can cause sciatica even though it is not a true radiculopathy.
5. The last cause of sciatica is Sacroiliac Joint Dysfunction which is not a true pinched nerve but can mimic the symptoms.
2. The second cause is Degenerative Disc Disease (DDD) as a result of aging and excessive micromotion of the spine over time. Bone spurs contribute as well.
3. Isthmic Spondylolisthesis is a result of a small stress fracture that allows one disc to slip forward over another disc which can also pinch a nerve. As the spinal canal narrows as we age and arthritis sets in, sciatica can occur.
4. The sciatica nerve runs behind the piriformis muscle of the buttock. If that muscle gets irritated, it can cause sciatica even though it is not a true radiculopathy.
5. The last cause of sciatica is Sacroiliac Joint Dysfunction which is not a true pinched nerve but can mimic the symptoms.
What Are the Symptoms of a Herniated Disc/Pinched Nerve?
Back pain is the most common complaint with a herniated disc or pinched nerve. This pain can be deep, penetrating, sharp, or throbbing. The onset of pain can be instantaneous, or it may be experienced as a snapping sensation in the back that is a result of an accidental tear of part of the fibrous part of the disc. The pain may radiate to other parts of the lower body affecting mobility and range of motion. Walking is difficult, and people may be appearing to limp to reduce the pressure on the painful side.
Right: Another view of a herniated disc pinching a nerve.
How is a Herniated Disc/Pinched Nerve Treated?
1. Taking it Easy
The treatment for most people with a herniated disc is usually conservative with bed rest, anti-inflammatory medications, and cold packs alternating with warm packs. Avoiding aggravating movements and activities with a slow return to normal activities is the key to long-term recovery. Too much sitting is bad because the sitting posture puts a large amount of stress and pressure on the lumbar spinal roots. Other medications include analgesics, muscle relaxants, or tranquilizers.
2. Physical Therapy & Traction Therapy
A qualified physiotherapist, chiropractor or osteopath can assist with decompression movements for the key area of your back, with exercises for strengthening core stability to support that area of your spine. Gentle spine traction (pulling apart) positions such as swimming can also greatly assist. Some specialty groups also offer computer and pulley assisted ‘Traction Table Therapy’ which can help manage the condition as well.
3. Spine Surgery for Pinched Nerve (Sciatica)
If a patient is not responding to conservative treatments mentioned above, then surgery may be required. Traditionally a spine surgeon might offer a microdiscectomy (a keyhole procedure performed through your back) to cut away the disc area which is compressing on the nerve. This is usually offered as a first surgery by spine surgeons.
Sometimes this type of discectomy surgery might only be a temporary solution to fix pain, because removing part of an unstable joint can cause greater instability, leading to more surgery in the future.
If conservative therapies fail and there is chance for permanent nerve damage, surgeons who are experienced in Cervical and Lumbar Disc Replacement using ‘new-generation’ implants such as the ESP or M6 Discs may recommend Artificial Disc Replacement right away, to restore healthy height and movement to their spine, giving the patient the best chance at a healthy lifestyle without concern for ongoing surgeries. Traditional spinal fusions using Robotic Navigation can also be offered as a ‘last line of defence’ for patients unsuitable for a motion-preserving surgery.
Surgery & Treatment for Sciatica (Pinched Nerve)
At Spine Connection we have regenerative and surgical treatments for all spine conditions. As every case is unique we encourage you to receive and compare opinions from our Neurosurgeon and Orthopedic Spine Specialists. We are here to help.
Begin My Assessment
Ask Our Doctors
Join Our Youtube Channel
Watch videos showcasing the latest technologies and surgery techniques, and keep up to date with patient stories from around the globe.